

TEAM LEADER : Alexandre Loupy
Mail : alexandre.loupy@inserm.fr
PHONE :
Localisation : Lab 359 – 3rd floor
DOCTORAL SCHOOL : ED 393: Santé publique, épidémiologie et sciences de l’information biomédicale – ED 157 BioSPC: Départment BCMPP

Our global aim is to accelerate the translation of immunological and gene expression discoveries into the clinical field of organ transplantation by filling the gap between basic science and applied biomedical researches. We will provide mechanistically driven pathogenesis of alloantibodies from in vitro cell models to murine models transferred to their clinical consequences in large prospective human cohorts in term of allograft injury, risk of failure and therapeutic strategies. Also, we will determine relevant and non-invasive biomarkers and identify rejection gene expression signatures in allografts.
We are developing a personalized approach of transplant medicine that will integrate multidimensional information deriving from classical histology and biology, clinical science together with novel information coming from ground breaking technologies in immunology, molecular biology, genetics and biomarkers. The present project has the ambitious but realistic goal to provide transplant clinicians with innovative and accessible tools for early prediction of individual risk of allograft rejection and transplant loss and offering them the possibility to personalize clinical management and treatment. The final product proposed by the present project is to build an integrated system in the form of a diagnostic/prognostic score.
This score will allow to make correlations with the conventional features of rejection and transplant pathology, improve the diagnostic accuracy, and provide mechanistic insights into exploring new pathways and operational biological processes involved in transplant rejection. This will also set the stage for personalized transplant medicine by providing end points for clinical trials with insights for therapy and patient clinical management.
The main objectives of our approach in transplantation and the iBox generation will be:
Follow us on twitter !
More information on our website
Our group is focused on risk stratification in the field of solid organ transplantation including large and accurately phenotyped cohorts of kidney, heart and lung transplant recipients.
Integrative epidemiology as a new field adapted for modern medical research
Over time, we have developed a particular scientific approach closely combining clinical investigations and statistics. The probabilistic mathematical tool is used in an integrative thinking approach, coupled at many levels with questions, insights and clinical investigations. We called this approach “integrative epidemiology”.
This approach received the “Grand Prix de l’Académie des Sciences 2013” in Paris (France). The rapid advances in medicine and sciences led to increased specialisation. The integrative epidemiology sets up an opposite approach where medical specialties and fundamental sciences are centralized around epidemiology.
The large quantity of information gathered from thousands of patients at multiple points in time result in a big data – smart data approach, and more importantly in a multidimensional approach.
Translational approach of solid organ transplantation
▸ The Paris Transplant Group is a multidisciplinary team dedicated to transplantation, which brings together immunologists, laboratory medical practitioners, researchers, nephrologists, cardiologists, pneumologists, pathologists, statisticians, and public health specialists.
▸ The team includes several referral transplant departments in kidney, heart and lung transplant, which are known as reference centres. Our consortium includes the leading national kidney transplant centre and the three leading Parisian kidney transplant teams, with 530 transplants executed on average each year.
The centres dedicated to heart transplant represent more than 80% of the overall national heart transplant activity (150 transplants executed on average each year) and the centre dedicated to lung transplant is the leader in Ile-de-France (75 transplants executed on average each year).
▸ During the past 8 years, the Paris Transplant Group has built an internationally recognized expertise in transplantation by studying the relationship between immune response and allograft injury in large cohorts. This strategy has recently been improved by the inclusion of new technologies regarding sensitive techniques for HLA antibodies characterization and gene expression assessment in allograft biopsies and new biomarkers discovery.
Integrative epidemiology vs. registries
So far, many results derive from large registries (UNOS in the US, Eurotransplant, National French Agency for Organ Procurment).
Despite their high value for descriptive purposes (prevalence and incidence), they lack information regarding phenotypes, histology, detailed immunology, allograft gene assessment, use of contemporary tests, and face wide heterogeneity in terms of management, patient care, and therapeutics. Registries and retrospective cohorts will never be able to go deep in pathogenesis, risk prediction and personalised transplant medicine given their current structuration.
Our approach uses exceptionally large prospective unselected cohorts with a very high level of detail (deep phenotyping), to test cutting-edge technologies with powerful and robust methodological tools. The historical transplant cohorts and the kidney, heart, and lung transplant cohorts of the Paris Transplant Group are unique worldwide.
During the last two years we have focused our research on:
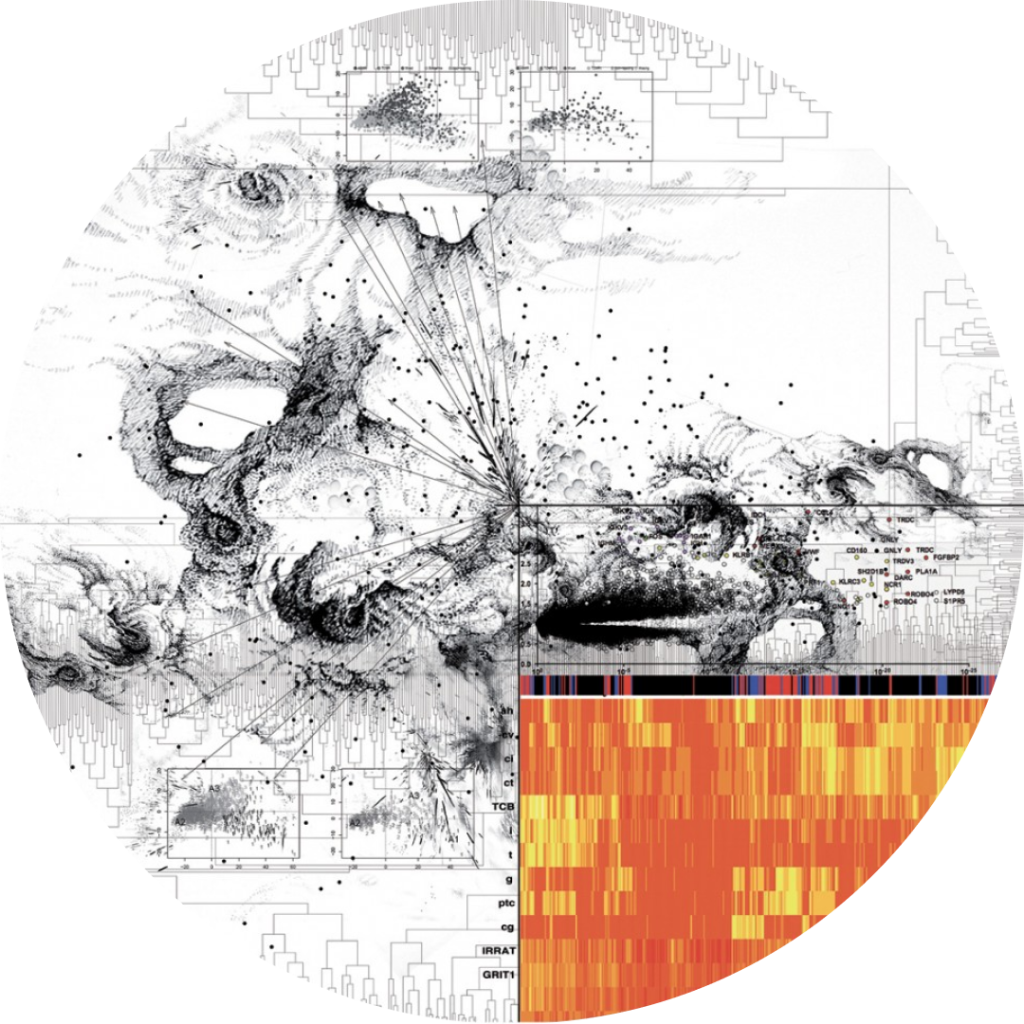
▸ The creation of a precision rejection diagnosis system applied in kidney, heart and lung transplant patients combining histology, clinical data and biology, using ground-breaking technologies in immunology, gene expression, and novel biomarkers.
As a proof of concept, we have already developed a score estimating the risk of allograft loss. This was obtained using a reference set of 5,000 kidney transplant patients recruited between 2004 and 2016 post-transplantation. This score includes clinical and biological data, allograft histopathology phenotyping, standardized patient management, timeline and kinetics.
It demonstrates fair performance for individual risk prediction of allograft loss at 7 years post-transplantation, in particular relatively high discrimination capacities (C statistics of 0.74), already outperforming prognostication systems adopted in the field of cancer. The score has been validated in transplant centres in Europe (Nantes, Toulouse, Lyon, Leuven) and United States (Johns Hopkins, Baltimore, Mayo clinic, Rochester) suggesting the exportability of our approach and results.
Of note, this score does not comprise new non-invasive immune and Omics markers.
▸ The discovery and study of new non-invasive biomarkers, for which we have provided robust data supporting clinical relevance.
▸ We were the first to demonstrate that donor specific anti-HLA antibodies and complement (C1q)-binding antibodies are major contributors to long-term allograft loss, leading to a 5 fold increase of graft loss rate at 7 years post-transplantation (NEJM 2013). This has been confirmed by numerous other teams in US and Europe.
▸ Post-transplantation monitoring of anti-HLA/DSA properties (C1q and IgG1,2,3,4 subclasses) demonstrates a significant added value for reclassification of the risk of allograft loss over the conventional assessment at the time of transplantation (JASN 2017).
▸ We have identified and validated robust blood and urine biomarkers of chronic allograft dysfunction/inflammation and operational tolerance (Circ 2017).
▸ The collaboration with the Alberta Transplant Applied Genomics Centre (ATAGC), which examines the molecular phenotype of disease states in humans in relationship to conventional phenotyping like histopathology and diagnostic imaging.
The ATAGC has specialized in genomics since 2010, and we are now able to use this technology and to transfer the already existing and validated molecular gene sets (http://atagc.med.ualberta.ca/Pages/default.aspx) to a diagnostic system comprising many other parameters included in the final iBox product.
We have already demonstrated the clinical relevance of biopsy gene expression profiling in many recent publications.
Teams of the consortium have shown that gene expression measurements in antibody-mediated rejection reflect pathophysiological pathways that can be targeted by specific therapeutics (JASN 2014).
Gene expression measurements reclassify 30% of antibody-mediated rejections beyond conventional features represented by histopathology (JASN 2014, Circ 2017).