

TEAM LEADER : Jean-Sébastien Hulot
Mail : jean-sebastien.hulot@inserm.fr
PHONE :+33 1 56 09 20 17
Localisation : Third Floor – Office: 362 – 369
DOCTORAL SCHOOL : ED 563 Médicament, Toxicologie, Chimie, Imageries « MTCI ». Paris Descartes, Sorbonne Paris Cité

Our team combines the work of internationally recognized and established teams that have come together to address the molecular, cellular and physiological mechanisms that lead to heart failure (with a growing focus on diastolic dysfunction) and to use this knowledge base to identify relevant targets to reverse the adverse remodeling process and eventually promote myocardial tissue repair.
For this purpose, the team develops approaches to preserve cardiac function with focus on arterial and myocardial stiffness, innovative modeling with iPS-derived cardiomyocytes and stem cell biology.
We follow three main research axes:
Keywords: heart failure, arterial stiffness, stem cells, iPSC, fibrosis, pharmacology

Heart failure (HF) is a major health problem in Western countries. The prevalence of symptomatic heart failure is estimated to be between 0.4% and 2.0% of the general population in Europe (Euro Heart Survey 2) and more than 1,000,000 people in France have heart failure. HF remains a leading cause of mortality and morbidity in Europe and its prevalence will continue to increase with the ageing population.
Most therapeutic developments have been achieved for people presenting with reduced left ventricular systolic function (so called HFrEF). However, it is estimated that up to half of heart failure patients present with a preserved ejection fraction (HFpEF) and this type of HF typically develops in ageing patients accounting for an increasing patient population. HFpEF patients present numerous comorbidities associated with adverse effects on cardiac and vascular functions including metabolic alterations (i.e., diabetes, obesity), arterial hypertension or kidney failure.
The pathophysiological mechanisms leading to HFpEF are poorly understood and no pharmacological options are currently available. At the biological level, several recent studies have shown that HFpEF results from cellular and molecular alterations that favor myocardial stiffness, that eventually lead to impaired cardiac and subsequent diastolic dysfunction. Several pathogenic factors have been recognized in contributing to increased left ventricular stiffness including microvascular dysfunction and rarefaction, excessive deposition of fibrotic components and increased cardiomyocyte passive stiffness.
The pathophysiological mechanisms leading to HFpEF are less understood but involve a progressive hypertrophic and fibrotic pathological remodeling of the heart in a pro-inflammatory context.
The team combines complementary expertise from three that decided to merge and start an this inter-disciplinary research program.
This project builds upon our previous developments, i.e. the demonstration of the value of arterial stiffness for stratifying the cardiovascular risk and potentially helping monitoring treatments, that will be further studied in the context of heart failure. We will explore whether increased aortic stiffness triggers and/or favors the development of diastolic dysfunction.
Increased arterial stiffness is indeed associated with significant changes in the arterial loading sequencing resulting in an early return of wave reflection. Reflected waves (i.e. backward travelling waves), which arrive in late systole, have little effect on peak myocardial stress, but rather on end-systolic stress. We will investigate this direct impact on the cardiac diastolic function in different settings.
In collaboration wuth the MEDES ((Institut de Médecine et de Physiologie Spatiales, in Toulouse), we are notably investigating cardiac changes in response to various conditions of arterial loading. This includes extreme situations such as conditions of low gravity. The French astronaut Thomas Pesquet has recently traveled to the ISS with an arterial tonometer developed together by ESSIE and our group.
In addition, we will expand arterial stiffness measurements in different groups of patients with cardiac diseases, notably patients with Heart failure with preserved ejection fraction.
Finally, we are actively collaborating to foster new techniques that allow a simple, non-invasive yet precise and reproducible measurement of tissue (ie, arterial and myocardial) stiffness in humans.
There is a limited predictive value of animal cardiac models (including large animals), especially regarding key cardiomyocytes components such as calcium cycling or diastolic function. There is thus a need for new experimental systems, ideally of human origin, which can model functional consequences and allow responses to therapeutic agents to be assessed.
Recent advances in stem cell biology now provide an unprecedented opportunity to study human cardiomyocytes, enabling us to elucidate the associations between genetic variability, disease susceptibility and key pathophysiological pathways at a level of detail previously unimaginable just a few years ago. In addition, human induced pluripotent stem cells (iPSCs) represent a powerful human model to study cardiac disease in vitro, notably channelopathies and sarcomeric cardiomyopathies.
During the last years, we have established a platform to generate and characterize human iPS cells. We have then developed reproducible and efficient small-molecule based protocols to differentiate hiPSC into ventricular cardiomyocytes.
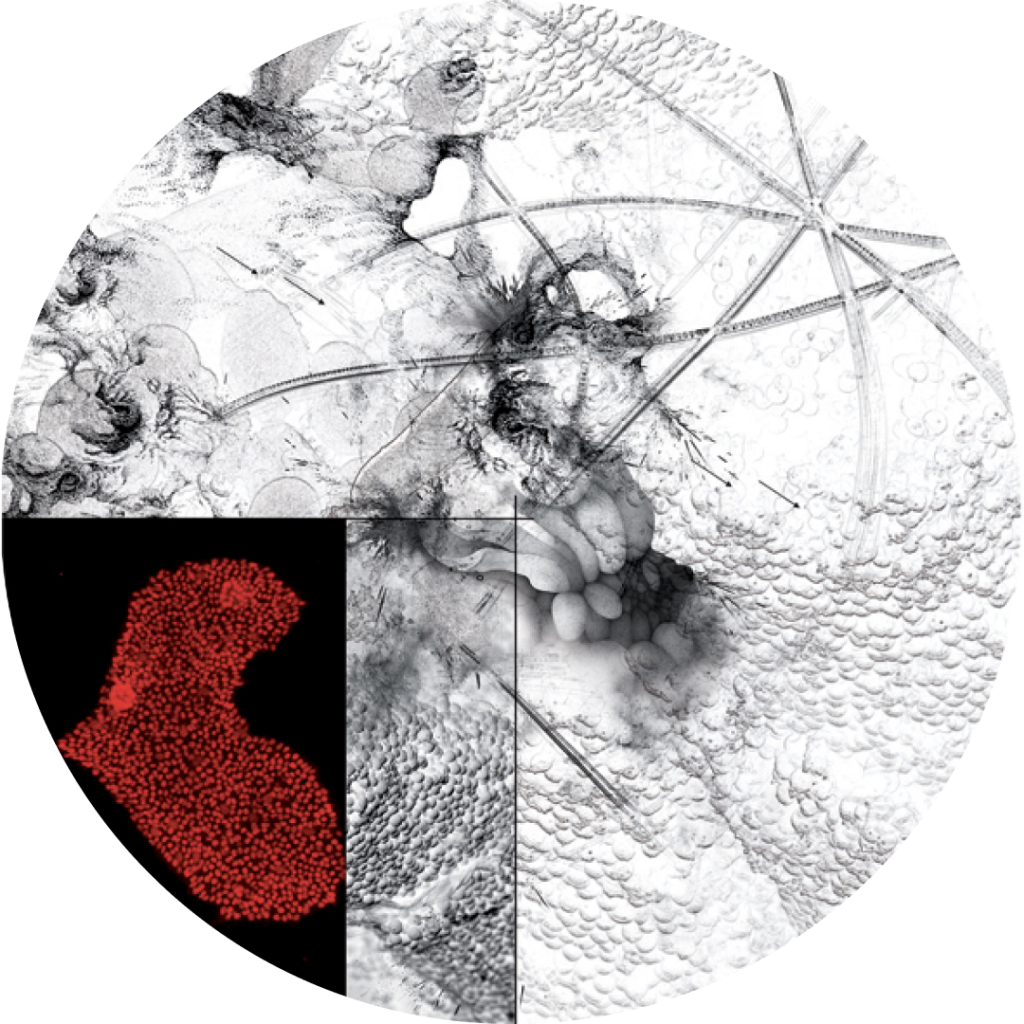
We have recently further developed these protocols by using epigenome interventions and micropatterning cell cultures (Figure 1). These approches are critical to provide iPS-derived cardiomyocytes with higher level of organisation and maturation.
These first steps are also critical for the development of future tools for disease modeling (especially cardiomyopathies), functional genomic studies or pharmacological assays. In collaboration biomedical engineers, we are developing new 3D engineered cardiac tissues using these pluripotent stem cells. These tissues form beating fibers that can then serve to measure parameters that reflect the contractile and relaxation phases.
In addition, we found that 3D cultures allow a better maturation of cardiomyocytes by forcing cell alignment and anisotropy. We showed that tissues can be used to reproduce the contractile defects associated with mutations affecting the calcium cycling and to measure the inotropic effects of drugs. In parallel, we have developed genome editing tools (based on CRISPR/Cas9) to directly target & modify genomic positions in the hiPSC clones therefore producing isogenic hiPSC clones.
We have also been able to demonstrate that hiPSC-CM can not only be useful to reproduce monogenic disoders but also to recapitulate more complex disorders, such as the predilection to cardiotoxic drug response of individual subjects.
We therefore developed and characterized a genetically diverse panel of subject-specific iPSCs that can be used as a cellular platform for testing individual drug reactions.
In addition, we used this library to further explore the molecular mechanisms underlying this predilection (using RNA-sequencing approaches) and found significant changes in expression of genes related to the regulation of cardiac electrical system.
These achievements will now be a critical support for further development of our new projects using human iPSC-based models to study determinants of cardiac diastolic dysfunction and cardiomyocytes stiffness.
We will also use this human cellular platform to test new metabolic interventions that have shown beneficial effects in murine models of heart failure. We will lastly develop new research programs investigating the use of patient-specific iPSC as a tool for precision medicine.
On top of cardiomyocytes, the heart contains multiple other cell types that can directly or indirectly interact with cardiomyocytes thereby representing an alternative way to promote cardiac tissue repair.
Among these cell types, we have been particularly focusing on cells with stem cell characteristics (in terms of self-renewal and multipotent capacity) that we found as resident cells in the myocardium.
The group co-directed by David Sassoon and Giovanna Marazzi focuses upon obtaining fundamental knowledge that can be translated to therapeutic approaches to target adult stem cells and the stem cell niche with the end goal of optimizing tissue regeneration.
A central project in our team is focused upon identifying genes that play a general role in multiple adult progenitor stem cells and therefore likely to play fundamental roles in stem cell behavior. This effort led to the identification of Pw1/Peg3, which we then showed to be involved in mediating cell stress responses.
The generation of a reporter mouse (PW1nLacZ, that expresses the nuclear β-galactosidase in the context of PW1 gene) then showed that Pw1/Peg3 is expressed in all adult progenitor cells examined to date, including the heart (Figure 2).
The presence of adult stem/progenitor cells within the myocardium has only been recently acknowledged and the function of these cells remains unclear. We used our PW1 reporter transgenic mouse to detect, isolate and characterize the PW1+ cells in normal and ischemic hearts.
Our results show that Pw1 is expressed in the interstitial cells of the heart and is not expressed in cardiac myocytes. In ischemic hearts, the number of PW1+ cells markedly increase suggesting that these cells participate in either injury and/or cardiac repair.
Cardiac PW1+ cells can be isolated and display both colony forming capacity and cell fate plasticity in vitro to form adipocytes, osteoblasts, chondrocytes, fibroblasts, endothelial and smooth muscle cells.
However, PW1+ colonies did not give rise to cardiomyocytes in vitro. Taking advantage of the high level and long-lasting expression of the β-gal reporter enzyme, we found that a significant proportion of fibroblasts were derived from PW1 expressing cells in ischemic hearts.
In contrast to adult hearts, the neonates present with a higher level of cardiac PW1+ cells that are capable of forming blood vessels.
We now propose a new paradigm where cardiac tissue fibrotic remodeling and microvascular rarefaction could originate from incompetent resident adult stem cells.
We are investigating the drivers of the cardiac PW1+ resident stem cells plasticity to a fibrogenic vs vasculogenic fate. We also develop a new metabolic intervention that favors the angiogenic potential of cardiac adult stem cells thus shifting them to a more competent role in cardiac tissue repair.