

TEAM LEADER : Bertrand Tavitian / Fabien Hyafil
Mail : bertrand.tavitian@inserm.fr / fabien.hyafil@aphp.fr
PHONE : +33 1 53 98 80 54
Localisation :
Lab: room 363, third floor
PET: room 379, third floor
MRI: room 445, fourth floor
DOCTORAL SCHOOL : ED 563 – Médicament-Toxicologie-Chimie-Imageries, Université Paris Cité

Our research encompasses many aspects of innovation in live imaging, from technologies for health to preclinical development, clinical trials and image treatment and analysis, with a special dedication to translational research. Our three major research domains are:
1) Image-guided mini-invasive therapy, especially Endoscopic tissue repair imaging, interventional radiology and Ultrasound therapy.
2) Discovery and validation of Imaging biomarkers for Cardiology, Oncology, vascular medicine and Atherosclerosis, using Artificial Intelligence as an important asset.
3) Hybrid multiparametric imaging, which includes translational MRI, imaging of cardiotoxicity, and hybrid imaging. We run preclinical computed tomography (CT), ultrafast ultrasound imaging (UUS), magnetic resonance imaging (MRI and positron emission tomography (PET), and clinical CT, UUS, MRI, PET).

1. IMAGE-GUIDED MINI-INVASIVE THERAPY
Offering the safety and logistic advantages of cell-free biotherapy, Extracellular Vesicles (EVs) derived from stem/stromal cells (SCs), are promising for regenerative medicine to promote tissue healing. We administered locally SC EVs embedded in a thermoresponsive gel, as a therapeutic strategy for managing post-surgical fistulas in a swine fistula model. This combination resulted in significant (i) reduction of fibrosis, (ii) decline of inflammatory response, (iii) decrease in myofibroblasts density, and (iv) increased angiogenesis. Our results present prospects for EV administration strategies and for the management of post-operative fistulas.
Image-guided chemo-embolization for suicide gene therapy:
In collaboration with the Centre de Recherche des Cordeliers, we developed a new intra-arterial treatment for liver tumor based on suicide gene therapy vectorized by mesenchymal stem cells injected into the tumor-feeding artery. Mesenchymal stem cells (MSCs) transduced by a gene encoding a cytochrome P450 isoenzyme (CYT2B6 *) metabolize Cyclophosphamide, leading to local cell death through a bystander effect. A proof of concept study in a VX2 liver tumor rabbit model showed near complete tumor eradication, without metastatic spread at 25 days, while the “gold standard chemoembolization treatment”, stabilized the tumor at 14 days but failed to prevent metastatic spread at 25 days.
Ultrasound therapy:
Ultrasound, applied in a focused and high-energy manner, can induce a cavitation phenomenon, a powerful tool for tissue modification. In the calcified aortic valve, ultrasound could allow the valve to become more flexible by fragmenting the calcifications. Our translational research project aims to understand the interactions between ultrasound and valve calcifications through an analysis of preclinical models (currently in pigs) and through a first clinical evaluation within the ongoing Valvosoft® study. We will develop the fundamental understanding of the mechanism of interactions between ultrasound and the heart valve through cooperation with Prof. R. Levine’s team in Boston. This project includes a broader field of vascular applications such as thrombus destruction that we are developing for the recanalization of venous thrombosis, with current in vitro and porcine model experiments (Messas et al Circulation 2021; ANR application in progress).
2. IMAGING BIOMARKERS, BIG DATA AND RADIOMICS
Cardiovascular perfusion and molecular imaging:
Our research is focused on improving the phenotyping of cardiovascular organs using quantitative perfusion imaging and molecular imaging. Our three major axes of research are:
1. Quantitative myocardial perfusion imaging with PET with perspectives of extending clinical applications of perfusion imaging to other organs than the heart;
2. Imaging of vulnerable atherosclerotic plaques with the development and validation of hybrid imaging of carotid plaques using a clinical PET-US system;
3. Assessing cardiac metabolism in inflammatory diseases and in oncology with FDG PET imaging.
The PACIFIC Project:
The prevalence of heart failure with preserved ejection fraction (HFpEF) is constantly increasing because of the aging of the population. It concerns about 50% of patients with heart failure and so far, treatments have not shown any therapeutic benefit. The PACIFIC project aims to evaluate several imaging biomarkers, in order to improve the classification of HFpEF and to better understand the phenotypic heterogeneity and evaluate new therapeutic approaches.
Cancer and Radiomics:
Recent developments in artificial intelligence applied to medical images accelerate biomarker discovery. Our team focuses on radiomics, the high throughput extraction of a large number of imaging features with no a priori hypothesis, applying machine learning and deep learning techniques to select the most clinically relevant imaging biomarkers. We used radiomics to predict malignancy in orbital tumors (Duron et al, Invest Radiol 2020), patient outcome in metastatic renal cell carcinoma and HPV status in head and neck cancers. We pay special attention to methodological issues such as the added information using multiple sequences in MRI (Lecler et al, Sci Rep 2019) and to the impact of image processing (Duron et al, PLoS One 2019).
3. HYBRID MULTIPARAMETRIC IMAGING
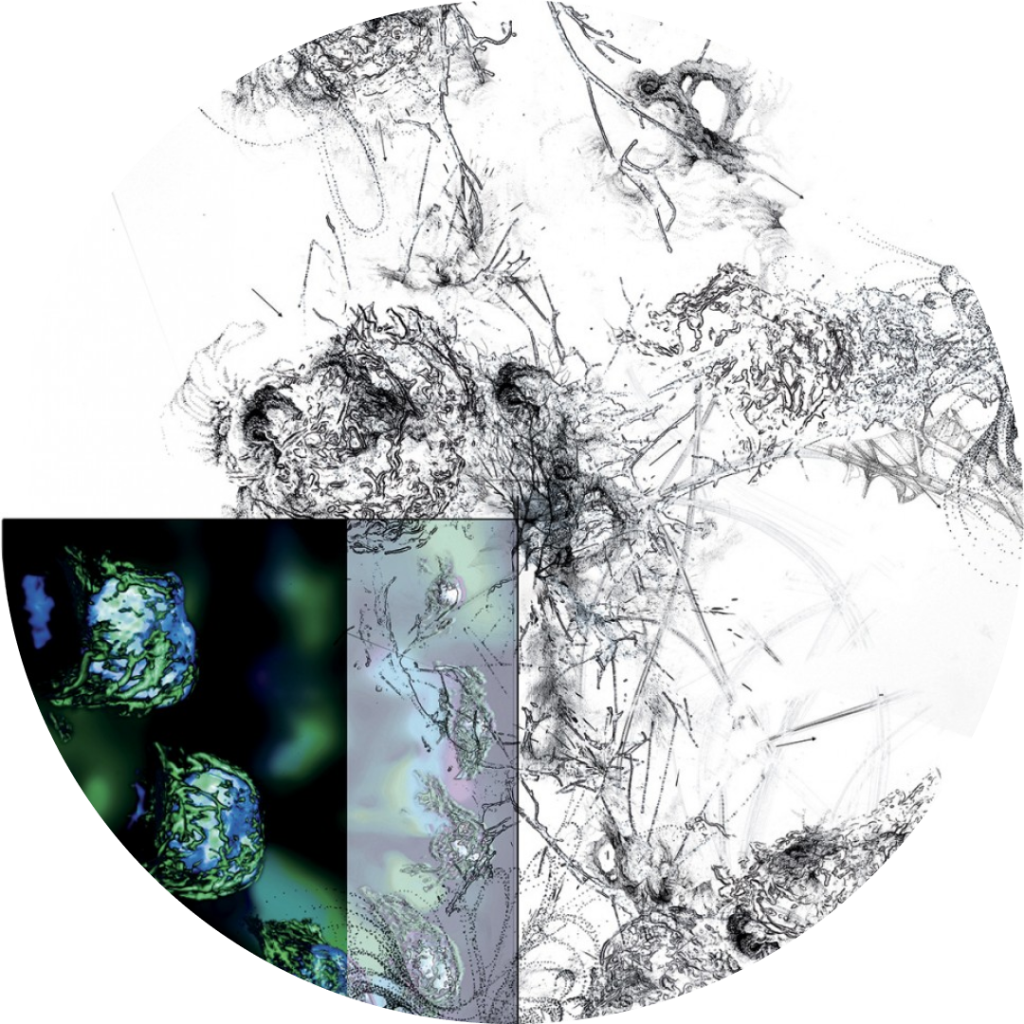
PET-Registered Ultrasound (PETRUS):
In collaboration with the team of Mickael Tanter at the Physics for Medicine department in Paris, we have recently introduced a new non-invasive in vivo preclinical imaging technology called PETRUS (PET-Registered-UltraSound), which merges positron emission tomography (PET) and ultrafast ultrasound imaging (UUI) (Provost et al. Nature Biomed Eng 2018; Perez-Liva et al. Phys Med Biol 2018). In preclinical studies, we have demonstrated the benefits of PETRUS in studying the interaction between tumor metabolism and vascular progression (Facchin et al. Theranostics, 2020). The complementarity of the performance and nature of information of each modality is excellent and allows to correct for blurring of cardiac PET images due to the motion of the heart (Perez-Liva et al. Mol Im Biol 2020).
