

TEAM LEADER : Maria-Christina Zennaro
Mail : maria-christina.zennaro@inserm.fr
PHONE : +33 1 53 98 80 42
Localisation : 1st floor, lab 175
DOCTORAL SCHOOL : ED BIO SORBONNE PARIS CITE

Arterial hypertension is the silent killer No. 1, accounting for >10 million deaths/year from stroke, ischemic heart disease, chronic kidney disease and other vascular causes. Detecting secondary forms of hypertension is key to targeted management and prevention of cardiovascular complications. Primary aldosteronism is the most common form of secondary hypertension, and aldosterone plays a major role in the regulation of blood pressure and electrolyte balance. The overall hypothesis of our research is that understanding the mechanisms responsible for aldosterone production and function will allow to improve diagnosis and treatment of arterial hypertension in the general population.
In this context, research performed by our team is entirely devoted to improve diagnosis and treatment of hypertension, by developing an integrative research program spanning from basic science in cell and animal models to genetic and clinical investigations in patients. The overarching aim of our program is to unravel the genetic and mechanistic architecture of blood pressure regulation in relation to aldosterone in order to generate knowledge translatable to clinics. Our vision is that understanding mechanisms driving inappropriate aldosterone production and its role in the pathophysiology of hypertension and cardiovascular complications is a critical gap in knowledge and unmet medical need. To achieve our goal, we apply the most recent genomic technologies on unique cohorts of patients with access to standardized clinical and biological information, tissue and DNA samples, integrated within national and international networks and programs. An original interdisciplinary approach combines complementary expertise in genetic and clinical investigation with high throughput genomic approaches, molecular, cellular and animal experiments. This approach has been extended to the development of multi-omics biomarker for patients with HT in the context of two EU-funded programs coordinated by MC Zennaro, the Horizon 2020 research and innovation project ENSAT-HT (www.ensat-ht.eu) and the Horizon Europe funded program HT-ADVANCE (www.ht-advance.eu).

The main aim of our research is to understand mechanisms driving inappropriate aldosterone production and its role in the pathophysiology of hypertension (HT) and cardiovascular complications to develop precision medicine in HT.
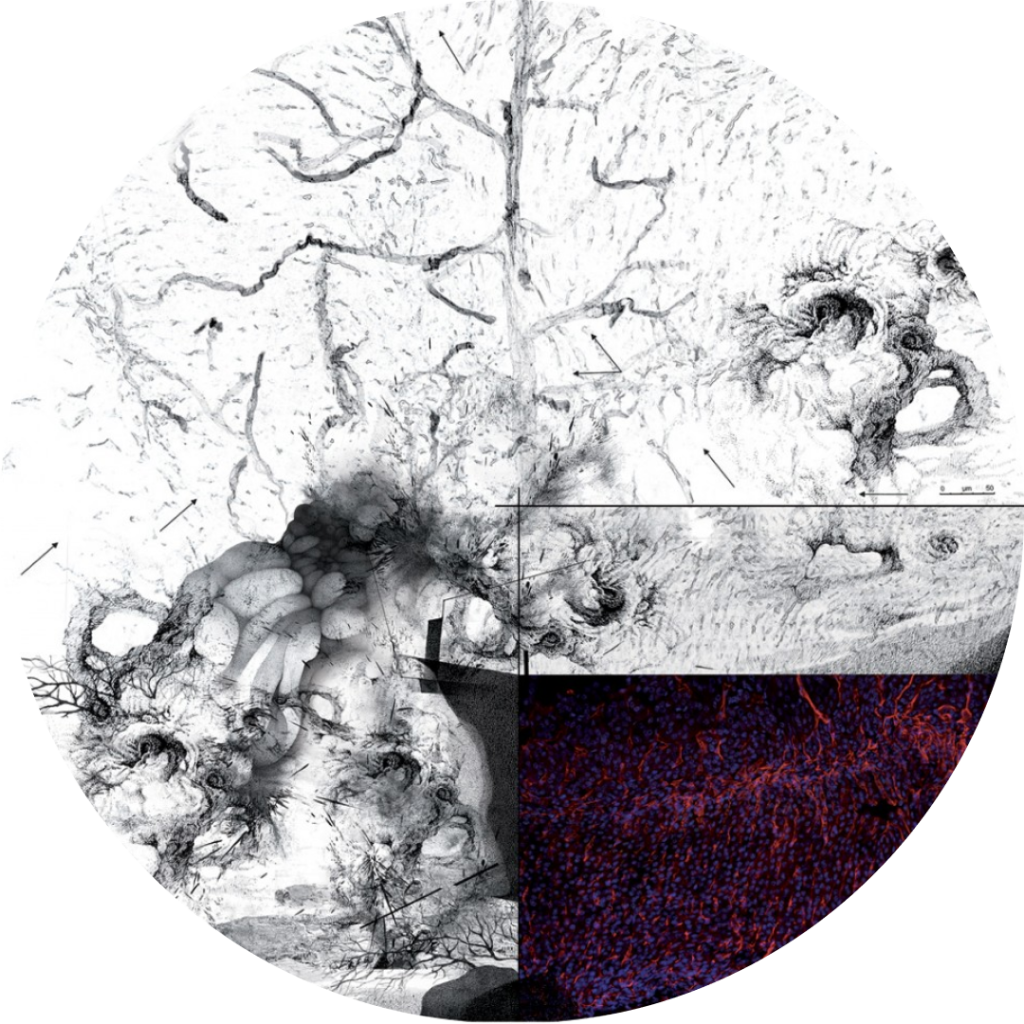
Arterial hypertension (HT) affects 40-50% of the population over 40 years old and is the most important risk factor for myocardial infarction, heart failure, stroke, cognitive disorders, end-stage renal disease and premature death. Although HT treatment can reduce incident adverse cardiovascular events, optimal blood pressure control is not being achieved in up to two thirds of patients. Detection of secondary forms of HT is key to targeted management of the underlying disease and prevention of cardiovascular complications. PA, due to autonomous aldosterone production from the adrenal gland due to an aldosterone producing adenoma (APA) or bilateral adrenal hyperplasia (BAH), is the most frequent form of secondary HT and its prevalence increases with HT severity, from ~5% in primary care to up to 25% in treatment-resistant HT. Due to the complexity of the work-up, fewer than 1% of patients are ever diagnosed and appropriately treated, thus contributing to a high burden of cardiovascular complications.
Our team has made major contributions to the knowledge of the genetic and pathogenic mechanisms of PA, revealing new genes responsible for familial and sporadic forms of the disease (Fernandes-Rosa et al, Nat Genet 2018, Zhou et al, Nat Genet 2021). More recently, we have performed the first GWAS study on PA that suggests that common genetic variation may underlie dysregulated aldosterone production in the general population, leading to PA in extreme cases (Le Floch et al, Nature communications 2022). The vision of the team has been extended from genetic and mechanistic studies to the development of omics-derived biomarkers for improved diagnosis and treatment of patients with hypertension.
Our current work addresses the following aims:
i) to understand how common genetic variation leads to dysregulated aldosterone production and hypertension;
ii) to improve treatment efficacy in hypertension by biomarker-guided personalised decision support (Horizon Europe HT-ADVANCE);
iii) to investigate pathogenic mechanisms of PA;
iv) to investigate the cardiometabolic consequences of inappropriate aldosterone levels.